Optimizing Bone Health- A Brief Introduction
In my world, bone health is a daily discussion in the adult population. During my time spent as a 1st and 2nd year consulting resident, roughly 20-30% of my hospital consultations were for osteoporotic insufficiency fractures. Osteoporotic insufficiency fractures include those of the vertebral body (compression fractures), distal radius, femoral neck, and sacrum. The mechanism of these injuries is often a mechanical ground level fall indicating a relatively low-energy mechanism that would under normal circumstances not cause fracture.
While I will reserve a discussion on the pathobiology of osteoporosis to another post, two of the most common questions I get from patients and facilities in the emergency room is “what should I have done to prevent this?” and “how can I prevent this from happening again?” While these are somewhat loaded questions, evidence would support the most effective methods are as follows:
Pharmacotherapy: includes medications such as bisphosphonates, which help to prevent bone resporption and anabolic agents such as Forteo, which function to help increase bone density (anabolic agents).
Nutritional support with Vitamin D, Calcium, and adequate protein intake.
Exercise and fall prevention training.
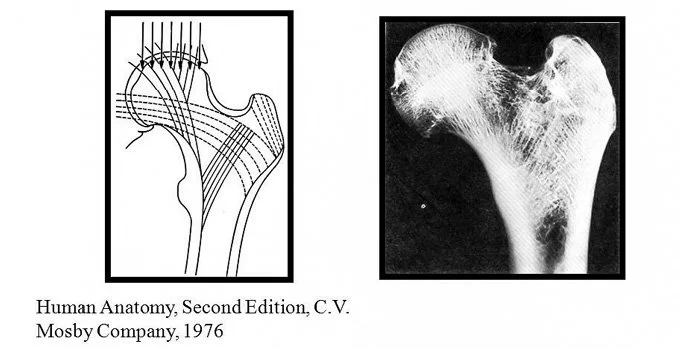
We will focus this article on number 3 above in this article. First off, why does load-bearing exercise help decrease progression of osteoporosis and risk for insufficiency fracture? The answer is explained by something called Wolff’s law. Julius Wolff was a German surgeon and anatomist who structured the bone microarchitecture in the 1800’s. What he noted was that a correlation existed between the orientation of the trabecular bone and mechanical stress lines. He eventually posited that bone will adapt to the mechanical loads by which it is placed. This work was expanded on in the 20th century, when Roux and Frost work established that bone is a dynamic organ that adapts to the demands placed on it (through loading). In summary, loading bone leads to bone formation and offloading bone leads to bone resorption. Today, Wolff’s principles remain a core principle in orthopaedics.
So, can this be applied to the management of osteoporosis? The available data would suggest that the answer is yes. This study published in the British journal of Sports Medicine (1) is a systematic review of 59 studies that compared physical activity with either no intervention as well as the effect of different doses and intensities of physical activity. Their data suggests that higher doses of activity are better (60+ mins, 2-3 times weekly), regular exercise can increase bone density in the both vertebral bodies and femoral neck, and resistance exercise appears to be the most effective modality of those studied. Further large systematic reviews on the topic are with similar findings. (2, 3) However, it should be noted that it does appear that different forms of exercise might be best to build bone mineral density in certain regions. For example, mind-body exercises such as Tai-Chi and Yoga may be best for the lumbar spine, while resistance training is likely the most effective in building bone density in the hip and distal radius.
Ultimately, none of this information is valuable unless it is applicable to folks daily lives. To me, it seems that the most important takeaway is that as one ages, it is vital to find a form of activity that is safe, challenging, enjoyable and sustainable. In a perfect world, this would likely involve some degree of cardiovascular training, resistance training and balance training with the use of supervised programs as needed (i.e. personal trainer). A general framework may look something like this:
Monday: 30-60 minutes of Aerobic training (Walking, biking, swimming)
Tuesday: Resistance training
Wednesday: Light aerobic activity (walk), Tai Chi, Yoga
Thursday: Resistance training
Friday: 30-60 minutes of Aerobic training
Saturday: Tai Chi, Yoga
Just some thoughts, feel free to share opinions and experiences below.
Until next time,
AD
https://link.springer.com/content/pdf/10.1186/s12966-020-01040-4.pdf
https://pubmed.ncbi.nlm.nih.gov/36355068/
https://pubmed.ncbi.nlm.nih.gov/34725872/